
Last updated on August 4th, 2024 at 05:52 pm
Sickle cell disease affects more than 100,000 people in the United States every year, and for three decades, Tesha Samuels was among them. After going through a gene therapy program funded by the National Heart, Lung, and Blood Institute (NHLBI), Samuels is in remission and relatively pain-free.
Pain is the most common complication of sickle cell disease. Sickle cells traveling through small blood vessels can get stuck and block blood flow throughout the body, which causes pain. Pain can occur in any part of the body, but commonly occurs in the hands, feet, chest, and back.
Now Samuels has a new outlook on life and is finally doing everything that sickle cell disease held her back from. She talked with NIH MedlinePlus Magazine about her experience with sickle cell disease and her life after treatment.
When and how were you diagnosed with sickle cell disease?
I was diagnosed in 1984 when I was 2 years old. I was born prior to the newborn screening mandate, so I wasn’t tested at birth. At the time, I had a lot of health issues my first couple years, and I visited the doctor’s office often. Finally, my mom took me to a physician who questioned if I had been tested for sickle cell disease. My mom didn’t know what sickle cell was at the time. Both my mom and I were tested. She tested positive as a carrier, and I tested positive for sickle cell disease. The trait for sickle cell is quite strong on my maternal side—my mother, grandmother, and great-grandmother all have it. But I’m the only one in my family who has sickle cell disease.
What symptoms did you first notice?
I was very young at the time of my diagnosis, but I remember it was very easy for me to catch a common cold or type of infection. As an infant, my mother told me that despite having all of the basic needs met like food and hygiene, it was very difficult to comfort me. She also noticed that I would wince when picked up. I believe that I was experiencing pain even as an infant.
As a toddler, she noticed I also fell down a lot but until the diagnosis, there wasn’t really an explanation. My family did a great job of helping and supporting before the diagnosis, but I can imagine it was difficult.
How did your diagnosis affect your day-to-day life?
When you have sickle cell disease, you always know you’re different. As a preteen and moving through my teenage years, I did a lot of masking. I masked the pain often, and I was in excruciating pain daily. Eventually you become numb, not to the pain, but the way you respond to the pain. Sometimes the pain can keep you in bed, but I didn’t make that an option for myself. Instead of allowing the pain to keep me in bed, I would ask myself, “What can I do to help myself feel normal? What can I do to have a sense of normalcy in my life?” I created routines that would help me respond to and cope with the pain. This routine carried me through my adult years. Most people I interacted with outside of my family didn’t know how much pain I was really in.
What was your treatment like before undergoing gene therapy?
My treatment plan included a lot of pain medication not necessarily because I desired it, but because I really needed it. Unfortunately, as time goes on, it feels like the medication isn’t as effective, so the dosage needed to achieve some level of relief needed to be increased. For me, the pain was so bad and deep that it could almost take my breath away if I didn’t have some pain medication to relieve it.
In addition to medication, blood transfusions were a part of my treatment. When I was 13, I had a transient ischemic attack (similar to a stroke). After that, I was doing routine blood transfusions to try to prevent that from happening again. The transfusions helped increase my hemoglobin (a protein in the blood that carries oxygen from the lungs to other organs) and hematocrit (the ratio of red blood cells to total blood volume). These provided more oxygen to the blood and gave me more energy. I would feel great for about two to three weeks, but of course, blood cells die off. I could literally feel my energy being depleted as my blood cells depleted. I did blood transfusions right up until the year I started undergoing gene therapy. I was doing monthly transfusions from age 13 to 36.
Can you describe your experience undergoing gene therapy?
Gene therapy was a beautiful blessing, but between the busulfan chemotherapy and the other medications they give you to help offset potential problems, the process was also very grueling. I was just really tired all the time. I had no energy. The great thing is that I have an amazing support system and my treatment was right before COVID-19, so I was able to have visitors. But just like sickle cell disease, no one can truly understand the feeling of undergoing the therapy. Regardless, I felt that if I could live with sickle cell disease for 36 years, then I could survive three months of treatment.
It was a painful daily process to allow the treatment to do its job. The pain was deep and sharp, and I was experiencing the effects of the chemotherapy. There were issues like the inability to swallow from my esophageal lining (in the tube that connects the throat and the stomach) being inflamed or having a terrible nosebleed from the busulfan.
There were a lot of processes to experience. From the medical processes of undergoing the treatment, to the process of going home and learning the new normal. It’s a transition from the physical to the mental. There’s a shift in both, and that’s a process that I grapple with daily. So, after living with this disease for 36 years, I now look forward to a life with new opportunities to finally do the things that I’ve always wanted to do. I’ve always had a zest for life, but it’s always been in the background. But now I can go full steam ahead with my goals and ambitions.
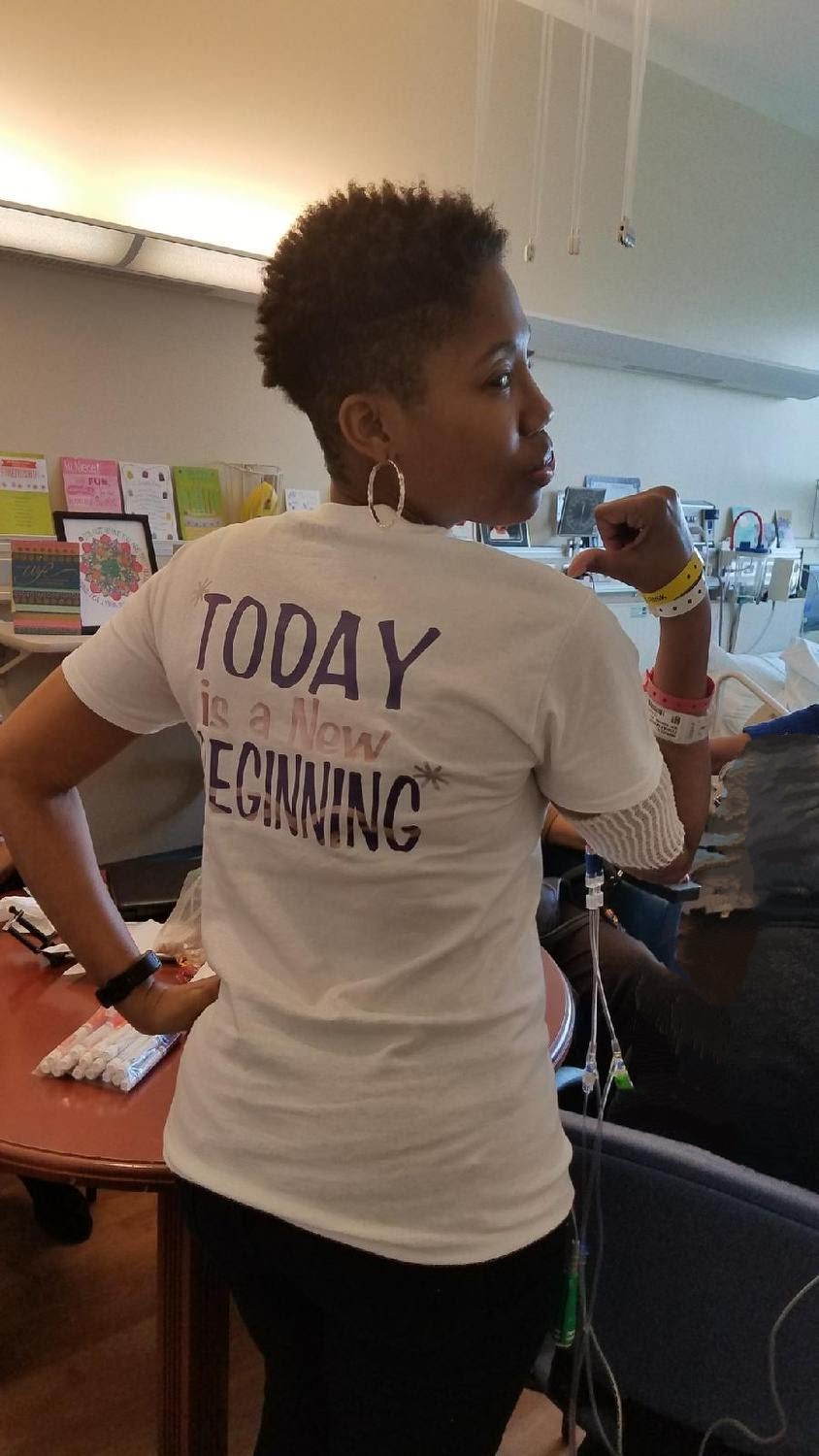
Tesha Samuels leans into advocacy to ensure that sickle cell illness doesn’t become a forgotten disease.
Since going into remission, do you still experience pain?
Very rarely, and when I do, I’m amazed that a simple over-the-counter medication is enough to be okay. I can just go to a regular drugstore, get ibuprofen, and be okay. When I do experience pain, I really try to understand that it’s “normal”, but nothing compared to what I’ve been accustomed to, and that’s truly a blessing.
In what ways do you advocate for others with sickle cell disease?
I speak at events, and I think doing interviews such as this are ways to advocate for others. I’m also in the process of getting my nonprofit off the ground. We just did our first annual Walk for ExSCellence, and we raised over $2,000 for the Sickle Cell Association of the National Capital Area Inc. and other organizations that look out for the well-being of people with sickle cell disease.
Sometimes I battle with survivors’ guilt because I wake up and feel completely different from how I did five years ago. I have a lot of friends who are still suffering and have tried different therapies with no results. It’s hard because here I am, finally doing some of the things that I’ve always wanted to do, and I feel like I’m leaving them behind. Life every day is advocacy.
