
Last updated on March 5th, 2025 at 09:00 am
December and January are peak months for respiratory syncytial virus (RSV) infections. While anyone can get RSV, severe infections are more common in young children and older adults. Fortunately, new vaccine approvals by the U.S. Food and Drug Administration (FDA) mean there are more options to avoid getting sick this winter.
In the spring of 2024, FDA licensed a new RSV vaccine, called MRESVIA, for adults 60 years of age and older. There are now three RSV vaccines recommended by the Centers for Disease Control and Prevention (CDC) for older adults—the other two are ABRYSVO and AREXVY.
Different RSV immunizations are recommended based on age, risk factors, and pregnancy. CDC recommendations are different from FDA approvals. Always check with your health care provider about what is right for you.
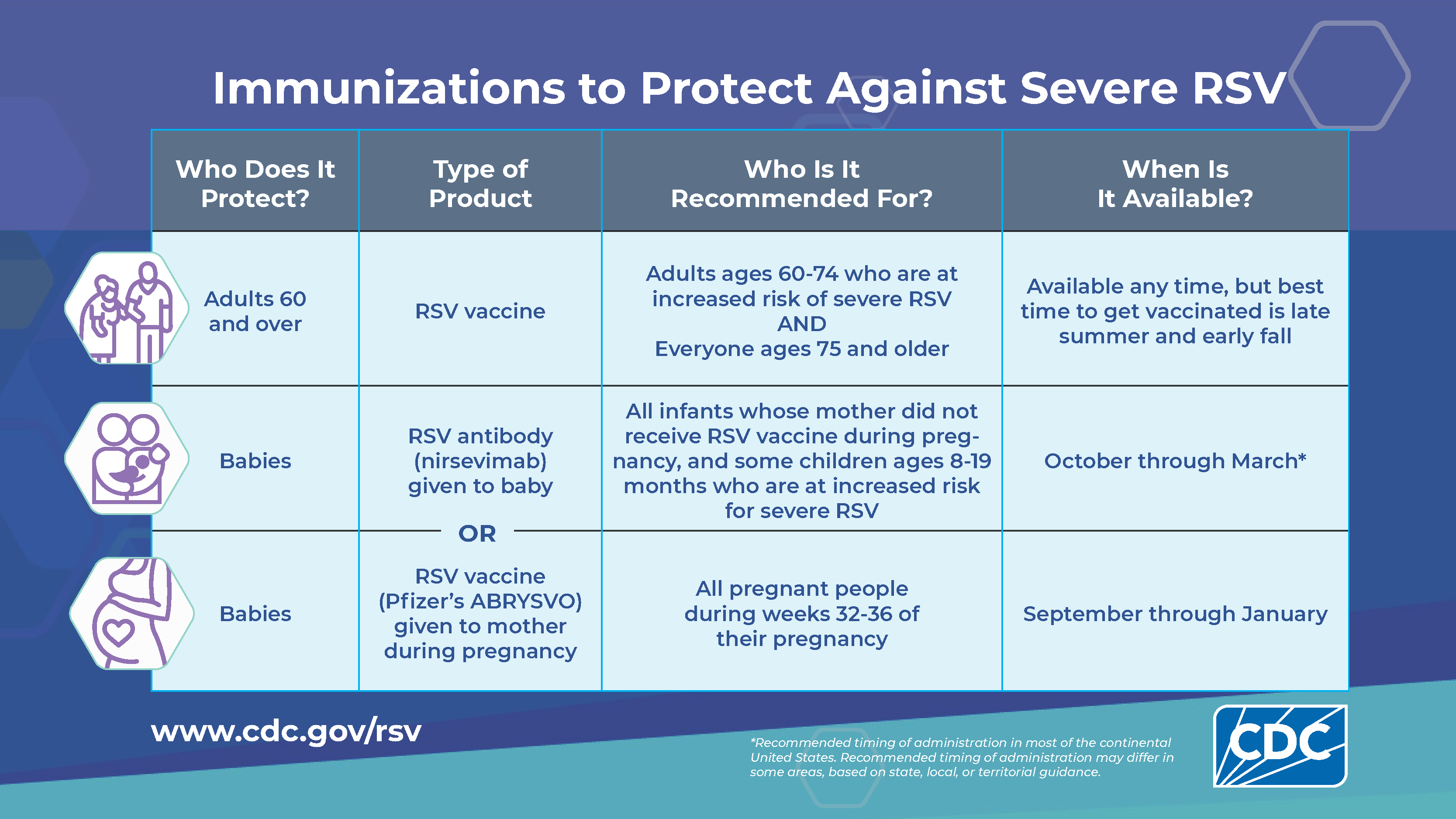
For larger image, click here.
What is RSV?
RSV is a highly contagious common respiratory virus. People of any age can get infected. It usually causes mild, cold-like symptoms.
RSV spreads from person to person directly, such as kissing the face of a child who has RSV, or indirectly, such as through the air by coughing and sneezing. You can also catch it by touching an object or surface with the virus on it before touching your mouth, nose, or eyes.
In the United States, RSV infections usually occur from fall through spring. People with RSV are generally contagious for three to eight days. But sometimes infants and people with weakened immune systems can continue to spread the virus for as long as four weeks.
While most cases are mild, it can cause serious lung infections in certain groups at higher risk, including:
- Infants
- Older adults, especially those ages 65 and older
- People with chronic medical conditions such as heart or lung disease
- People with weakened immune systems
What are the symptoms?
Symptoms of RSV infection usually start about four to six days after infection and may mimic the common cold:
- Runny nose
- Decrease in appetite
- Cough
- Sneezing
- Fever
- Wheezing
- Trouble breathing
These symptoms usually appear in stages instead of all at once. In very young infants, the only symptoms may be irritability, decreased activity, and trouble breathing. RSV can also cause more severe infections, especially in people at high risk. These infections include bronchiolitis, an inflammation of the small airways in the lung, and pneumonia, an infection of the lungs. If symptoms get worse over time, see a doctor right away.
How is it diagnosed?
A doctor can diagnose RSV. They can do tests, such as X-rays and blood or urine tests, to check for complications in people with severe infections. A doctor can also order lab tests, but they are usually for people with severe infections.

Young children and infants with severe RSV infections may require hospitalization.
How is RSV treated?
There is no specific treatment for RSV, but most people get better on their own in a week or two. Drink lots of fluid to prevent dehydration. You can take over-the-counter pain relievers for fever or pain, but do not give aspirin to children. And do not give cough medicine to children younger than 4 years old.
How is RSV prevented?
To avoid catching RSV, wash your hands often with soap and water for at least 20 seconds or use sanitizer hand gel that contains at least 60% alcohol. Getting one of the available vaccines if you are eligible is also an effective way to lower your risk of RSV disease.
RSV can survive for many hours on hard surfaces, such as tables and crib rails. It typically lives on soft surfaces, such as tissues and hands, for shorter amounts of time.
The CDC recommends everyone ages 75 and older (and adults ages 60 to 74 who are at increased risk of severe infection) get an RSV vaccine. Pregnant people during their 32nd through 36th week of pregnancy are also advised to get the ABRYSVO vaccine. Young infants whose mothers did not receive one during pregnancy can receive a protective RSV antibody (different from a vaccine). Talk with your health care provider about the best time to get your vaccine. If you have already gotten an RSV vaccine, you do not need to get another one.
RSV vaccines are usually covered by private health insurance, the Children’s Health Insurance Program, Medicare Part D, Medicaid, and TRICARE for military. CDC’s Vaccines for Children program also provides free immunizations for children at participating doctor’s offices, pharmacies, and health clinics.
